Passive Immunotherapy
Passive Immunotherapy
Active immunotherapies:
Cytokines (TNFa IL-2, IFNs)
Cancer vaccines
tumour CTL and APC
DC priming
Passive immunotherapy:
Administration of monocolnal (clone derived asexually from a single individual or cell) antibodies which target either tumour-specific or over expressed antigens
Generally comprised of antibodies made outside of the body (in a lab)
administered to patients to provide immunity against a disease, or to help fight existing disease
do not stimulate a patient’s body to ‘actively’ respond to a disease the way a vaccine does
immunogen is given several times to induce a strong secondary response
blood serum contains many different antibodies to the immunogen
most immunogens have multiple antigenic epitopes
each stimulates a different B cell clone/receptor –> polyclonal antibody (PAb) response

Monoclonal antibody (mAb) therapy is the most widely used form of cancer immunotherapy. Monoclonal antibodies cannot be purified from a polyclonal sample and are derived from a single clone/specific for a single epitope.

Antibodies in cancer therapy:
Trigger immune system to attack cancer cells
Block molecules that stop the immune system working (checkpoint inhibitors)
Block signals telling cancer cells to divide
Carry drugs or radiation to cancer cells
Checkpoint inhibitors
Immune system uses particular molecules to stop it being over activated and damaging healthy cells - these are known as checkpoints
some cancers make high levels of checkpoint molecules to switch of immune system T cells which would normally attack cancer cells
examples of targets include CTLA-4, PD-1 and PD-L1 (programmed death ligand 1)

Blocking cell division signals
Cancer cells often express large amounts of growth factor receptors on their surface –> rapid cell division when growth factors stimulate them
some monoclonal antibodies stop growth factor receptors working
either by blocking the signal or the receptor itself
cancer no longer gets signal to divide

Carrying drugs/radiation
drugs or radioisotopes can be attached to monoclonal antibodies
the mAB binds to the cancer cell, delivering directly
known as conjugated MABs

More Posts from T-b-a-blr-blog and Others
How to remember Lysteria monocytogenes tumbling motility?
MICROBIOLOGY MNEMONIC
So, Lysteria rhymes with Hysteria, and when I think of hysteria I think of someone dancing Hysterically…..(actually, me dancing hysterically..)
I also googled Hysteria, and found this:

HYSTERIA RADIO!
So here it goes: “Lysteria dances to Hysteria Radio”
If I don’t come up with all these silly associations my brain melts and confuses all the freakin bacterias, so bear with me…

Hello everyone, welcome to my latest 4-part series to help you land that job after uni! This series will cover what to do before, during, and after a job interview to ensure you leave a positive impression on the interviewers and hopefully help you cinch opportunities! Enjoy!
How To Set Your Career On The Right Path Before You Even Graduate! (Link) Part 2: During The Interview (Link) Part 3: After The Interview (Link)
Research the job position and company values.
It is critical to tackle all the requirements in your cover letter as well as your resume, and to be able to answer questions in the interview in a way that highlights you have those values the company is seeking. Even if the company doesn’t have a public ad, research similar positions at different companies and read those job descriptions. Have situations you’ve dealt with in your arsenal for answering situational questions.
Make sure your resume is updated perfectly.
It’ll save you a lot of time if you just update your resume every time you start something new! Standard stuff: Use ‘clean’ standard fonts, white A4 paper, single sided, 2 cohesive colours max. Include at least the minimum components or a combination of them: the rough order should be:
Career Objective
Education
Relevant Experience (include key responsibilities and noteworthy performance points)
Extra-Curricular Activities (if relevant)
Skills
Referees (usually just write “available on request”)
Cold call!
This is how I got my first relevant job as an optical assistant, which in a way, led to my current position today. Even whilst I was working as an optical assistant, occasionally we would get a new hire if their resume seemed good and they interviewed well.
Prepare for common interview questions.
Have scenarios ready illustrating how you dealt with a difficult situation

Who wants a box of chocolates when you can have a petri dish of bacteria?
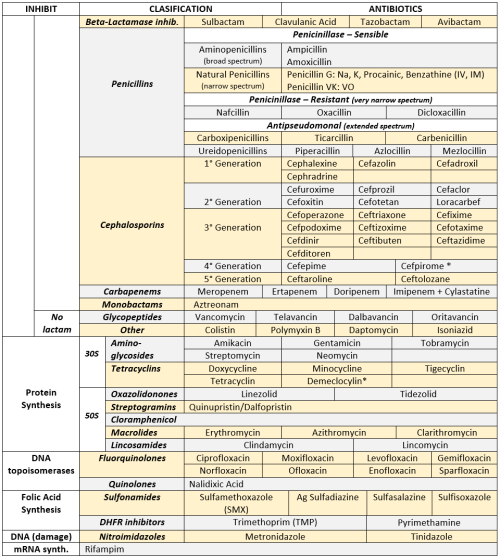
ANTIBIOTICS CHEAT SHEET :)
Also, REMEMBER!!!!
* Sulfonamides compete for albumin with:
Bilirrubin: given in 2°,3°T, high risk or indirect hyperBb and kernicterus in premies
Warfarin: increases toxicity: bleeding
* Beta-lactamase (penicinillase) Suceptible:
Natural Penicillins (G, V, F, K)
Aminopenicillins (Amoxicillin, Ampicillin)
Antipseudomonal Penicillins (Ticarcillin, Piperacillin)
* Beta-lactamase (penicinillase) Resistant:
Oxacillin, Nafcillin, Dicloxacillin
3°G, 4°G Cephalosporins
Carbapenems
Monobactams
Beta-lactamase inhibitors
* Penicillins enhanced with:
Clavulanic acid & Sulbactam (both are suicide inhibitors, they inhibit beta-lactamase)
Aminoglycosides (against enterococcus and psedomonas)
* Aminoglycosides enhanced with Aztreonam
* Penicillins: renal clearance EXCEPT Oxacillin & Nafcillin (bile)
* Cephalosporines: renal clearance EXCEPT Cefoperazone & Cefrtriaxone (bile)
* Both inhibited by Probenecid during tubular secretion.
* 2°G Cephalosporines: none cross BBB except Cefuroxime
* 3°G Cephalosporines: all cross BBB except Cefoperazone bc is highly highly lipid soluble, so is protein bound in plasma, therefore it doesn’t cross BBB.
* Cephalosporines are "LAME“ bc they do not cover this organisms
L isteria monocytogenes
A typicals (Mycoplasma, Chlamydia)
M RSA (except Ceftaroline, 5°G)
E nterococci

* Disulfiram-like effect: Cefotetan & Cefoperazone (mnemonic)
* Cefoperanzone: all the exceptions!!!
All 3°G cephalosporins cross the BBB except Cefoperazone.
All cephalosporins are renal cleared, except Cefoperazone.
Disulfiram-like effect
* Against Pseudomonas:
3°G Cef taz idime (taz taz taz taz)
4°G Cefepime, Cefpirome (not available in the USA)
Antipseudomonal penicillins
Aminoglycosides (synergy with beta-lactams)
Aztreonam (pseudomonal sepsis)
* Covers MRSA: Ceftaroline (rhymes w/ Caroline, Caroline the 5°G Ceph), Vancomycin, Daptomycin, Linezolid, Tigecycline.
* Covers VRSA: Linezolid, Dalfopristin/Quinupristin
* Aminoglycosides: decrease release of ACh in synapse and act as a Neuromuscular blocker, this is why it enhances effects of muscle relaxants.
* DEMECLOCYCLINE: tetracycline that’s not used as an AB, it is used as tx of SIADH to cause Nephrogenic Diabetes Insipidus (inhibits the V2 receptor in collecting ducts)
* Phototoxicity: Q ue S T ion?
Q uinolones
Sulfonamides
T etracyclines

* p450 inhibitors: Cloramphenicol, Macrolides (except Azithromycin), Sulfonamides
* Macrolides SE: Motilin stimulation, QT prolongation, reversible deafness, eosinophilia, cholestatic hepatitis
* Bactericidal: beta-lactams (penicillins, cephalosporins, monobactams, carbapenems), aminoglycosides, fluorquinolones, metronidazole.
* Baceriostatic: tetracyclins, streptogramins, chloramphenicol, lincosamides, oxazolidonones, macrolides, sulfonamides, DHFR inhibitors.
* Pseudomembranous colitis: Ampicillin, Amoxicillin, Clindamycin, Lincomycin.
* QT prolongation: macrolides, sometimes fluoroquinolones

Pneumonia & Meningitis Timelines

Me durning finals.
CYSTIC FRIBROSIS
G511D mutation: missense mutation, Glycine replaced by Aspartate.
Only 5% of pts with CF have this mutation.
Defective channel opening or gating.
IVACAFTOR: new drug, acts directly in the CFTR channel, opens it up. First drug that afects the ethiology :)
Trade name: Kalydeco

PSEUDOmonas aeroginosa.
Pneumonia
Sepsis (black lesion on skin).
External otitis (swimmers ear)
UTI,Drug use .
Diabetic osteomylitis
Aminoglycoside„,extended spectrum penicillin(pipracilin,ticarcillin)
Think pseudomonas in burn victims
Microbiology Mnemonic
STD: Chlamydia Trachomatis’ serotypes
“Eye Don't Know why people don’t use condoms”
Most common BACTERIAL STD in the US
Serotypes: D-K : nongonococcal urethritis, cervicitis, PID
Eye: Inclusion conjunctivitis.
Pneumonia (staccato cough) / Inclussion conjunctivitis in neonates / infants

STD: L imphogranuloma Venereum
L1,2,3
Africa, Asia, South America
Swollen lymph nodes, ulcers, fistulas -> Genital elephantiasis

tr AC homa
A-C serotypes (A,B,Ba,C)
Follicular conjuntivitis -> Conjuntival scarring -> inturned eyelashes -> corneal scarring -> BLINDNESS


Cryptosporidium
Cryptosporidium is a microscopic parasite that causes the diarrhoeal disease cryptosporidiosis. Both the parasite and the disease are commonly known as “Crypto.”
The parasite is protected by an outer shell (oocyst)
Allows survival outside the body for long periods of time
Very tolerant to chlorine disinfection.
Water is the most common form of spread
Poses serious risk to immunocompromised individuals, eg AIDS; cancer and transplant patients who are taking certain immunosuppressive drugs.

Symptoms
Symptoms of cryptosporidiosis generally begin 2 to 10 days (average 7 days) after infection.
Watery diarrhea
Stomach cramps or pain
Dehydration
Nausea
Vomiting
Fever
Weight loss
Some people with Crypto will have no symptoms at all.
Symptoms usually last about 1 to 2 weeks (with a range of a few days to 4 or more weeks) in persons with healthy immune systems. Occasionally, people may experience a recurrence of symptoms after a brief period of recovery before the illness ends. Symptoms can come and go for up to 30 days.
In immunocompromised persons Cryptosporidium infections could possibly affect other areas of the digestive tract or the respiratory tract.
Diagnosis & Detection

Cryptosporidium oocysts in a modified acid-fast stain. (CDC Photo; DPDx)
Examination of stool samples.
Detection can be difficult - several stool samples over several days.
acid-fast staining, direct fluorescent antibody [DFA] , and/or enzyme immunoassays
Molecular methods (e.g., polymerase chain reaction – PCR) are increasingly used in reference diagnostic labs,
Treatment
Most people who have healthy immune systems will recover without treatment. Young children and pregnant women may be more susceptible to dehydration resulting from diarrhoea.
For those persons with AIDS, anti-retroviral therapy (improves the immune status) will also decrease or eliminate symptoms of cryptosporidiosis. However, even if symptoms disappear, cryptosporidiosis is often not curable and the symptoms may return if the immune status worsens.
Cryptosporidium and AIDS
Advanced immunosuppression — typically CD4 T lymphocyte cell (CD4) counts of <100 cells/µL — is associated with the greatest risk for prolonged, severe, or extraintestinal cryptosporidiosis.
The three species that most commonly infect humans are Cryptosporidium hominis, Cryptosporidium parvum, and Cryptosporidium meleagridis. Infections are usually caused by one species, but a mixed infection is possible.
Up to 74% of diarrhoea stools in AIDS patients demonstrating the organism in less developed countries where potent antiretroviral therapy is not widely available,
cryptosporidiosis has decreased and occurs at an incidence of <1 case per 1000 person-years in patients with AIDS.4 Infection occurs through ingestion of Cryptosporidium oocysts. Viable oocysts in feces can be transmitted directly through contact with infected humans or animals, particularly those with diarrhea. Oocysts can contaminate recreational water sources such as swimming pools and lakes, and public water supplies and may persist despite standard chlorination (see Appendix: Food and Water-Related Exposures). Person-to-person transmission is common, especially among sexually active men who have sex with men.
Fever is present in approximately one-third of patients and malabsorption is common.
The epithelium of the biliary tract and the pancreatic duct can be infected with Cryptosporidium, leading to sclerosing cholangitis and to pancreatitis secondary to papillary stenosis,
Pulmonary infections also have been reported, and may be under-recognized.
Treatment
ART with immune restoration to a CD4 count >100 cells/µL usually leads to resolution
Treatment of diarrhoea with anti-motility agents (AIII) may be necessary.
Patients with biliary tract involvement may require endoscopic retrograde choledocoduodenoscopy for diagnosis.
Immune reconstitution inflammatory syndrome (IRIS) has not been described in association with treatment of cryptosporidiosis.
No pharmacologic interventions are known to be effective in preventing the recurrence of cryptosporidiosis.
No therapy has been shown to be effective without ART.
-
 kosmonautika liked this · 4 years ago
kosmonautika liked this · 4 years ago -
 forensicfiless reblogged this · 4 years ago
forensicfiless reblogged this · 4 years ago -
 visander liked this · 4 years ago
visander liked this · 4 years ago -
 052955 liked this · 4 years ago
052955 liked this · 4 years ago -
 260215 liked this · 5 years ago
260215 liked this · 5 years ago -
 pizza-and-studying liked this · 6 years ago
pizza-and-studying liked this · 6 years ago -
 shabbytigers liked this · 6 years ago
shabbytigers liked this · 6 years ago -
 mermaidmountaineer-blog reblogged this · 6 years ago
mermaidmountaineer-blog reblogged this · 6 years ago -
 erin-spradlin-blog reblogged this · 6 years ago
erin-spradlin-blog reblogged this · 6 years ago -
 whiteladybibleschool reblogged this · 6 years ago
whiteladybibleschool reblogged this · 6 years ago -
 myownstudystuff reblogged this · 6 years ago
myownstudystuff reblogged this · 6 years ago -
 myownstudystuff reblogged this · 6 years ago
myownstudystuff reblogged this · 6 years ago -
 heermione liked this · 6 years ago
heermione liked this · 6 years ago -
 specskitty-blog reblogged this · 6 years ago
specskitty-blog reblogged this · 6 years ago -
 joyaless liked this · 6 years ago
joyaless liked this · 6 years ago -
 maxalexenko-blog reblogged this · 6 years ago
maxalexenko-blog reblogged this · 6 years ago -
 t-b-a-blr-blog reblogged this · 6 years ago
t-b-a-blr-blog reblogged this · 6 years ago -
 t-b-a-blr-blog liked this · 6 years ago
t-b-a-blr-blog liked this · 6 years ago -
 that-works liked this · 7 years ago
that-works liked this · 7 years ago -
 ffbuddy68 liked this · 7 years ago
ffbuddy68 liked this · 7 years ago -
 sweet-wake-up liked this · 7 years ago
sweet-wake-up liked this · 7 years ago -
 med8dicted reblogged this · 7 years ago
med8dicted reblogged this · 7 years ago -
 queen-elizabeth-the-3st liked this · 7 years ago
queen-elizabeth-the-3st liked this · 7 years ago -
 xxjanedoexd reblogged this · 7 years ago
xxjanedoexd reblogged this · 7 years ago -
 lucydragoneelnatsu liked this · 7 years ago
lucydragoneelnatsu liked this · 7 years ago -
 thatburnsguy liked this · 7 years ago
thatburnsguy liked this · 7 years ago -
 tercbutil liked this · 7 years ago
tercbutil liked this · 7 years ago -
 tercbutil reblogged this · 7 years ago
tercbutil reblogged this · 7 years ago -
 sussantos reblogged this · 7 years ago
sussantos reblogged this · 7 years ago -
 reemees-blog liked this · 7 years ago
reemees-blog liked this · 7 years ago -
 heartsyy liked this · 7 years ago
heartsyy liked this · 7 years ago -
 lattenursing liked this · 7 years ago
lattenursing liked this · 7 years ago -
 wildfuckrebel reblogged this · 7 years ago
wildfuckrebel reblogged this · 7 years ago -
 empresslaurosaurus reblogged this · 7 years ago
empresslaurosaurus reblogged this · 7 years ago -
 sco-fi reblogged this · 7 years ago
sco-fi reblogged this · 7 years ago -
 shinladyanarki reblogged this · 7 years ago
shinladyanarki reblogged this · 7 years ago