Hope It Helps @shreeparn :)


Hope it helps @shreeparn :)
More Posts from T-b-a-blr-blog and Others

Positives are violet in color and negatives are red or pink on gram stain! My untidy handwritten notes here.
Antibodies (Human)

The ‘foot’ (bottom) of the antibody is known as the Fc fragment - binds to cells, binds to complement = effector function (kills or removes antigen)
The top (antigen binding) is the Fab fragment
Chains are held together with disulphide binds
Associated molecules allow intracellular signalling
Normally 3X constant heavy chain domains per chain and a hinge region (except μ and ε which have 4 and no hinge region)
Classes of Immunoglobulins
The five primary classes of immunoglobulins are IgG, IgM, IgA, IgD and IgE, distinguished by the type of heavy chain found in the molecule.
IgG - gamma-chains
IgMs - mu-chains
IgAs - alpha-chains
IgEs - epsilon-chains
IgDs - delta-chains.
Differences in heavy chain polypeptides allow different types of immune responses. The differences are found primarily in the Fc fragment. There are only two main types of light chains: kappa (κ) and lambda (λ), and any antibody can have any combination of these 2 (variation).
IgG
monomer
Gamma chains
70-85% of Ig in human serum.
secondary immune response
only class that can cross the placenta - protection of the newborn during first 6 months of life
principle antibody used in immunological research and clinical diagnostics
21 day half life
Hinge region (allows it to make Y and T shapes - increasing chance of being able to bind to more than one site)
Fc strongly binds to Fcγ receptor on phagocyte - opsono-phagocytosis
Activates complement pathway

IgM
Serum = pentamer
Primary immune responses - first Ig to be synthesised
complement fixing
10% of serum Ig
also expressed on the plasma membrane of B lymphocytes as a monomer - B cell antigen receptor
H chains each contain an additional hydrophobic domain for anchoring in the membrane
Monomers are bound together by disulfide bonds and a joining (J) chain.
Each of the five monomers = two light chains (either kappa or lambda) and two mu heavy chains.
heavy chain = one variable and four constant regions (no hinge region)
can cause cell agglutination as a result of recognition of epitopes on invading microorganisms. This antibody-antigen immune complex is then destroyed by complement fixation or receptor mediated endocytosis by macrophages.
In humans there are four subclasses of IgG: IgG1, IgG2, IgG3 and IgG4. IgG1 and IgG3 activate complement.

IgD
B cell receptor
<1% of blood serum Ig
has tail pieces that anchor it across B cell membrane
forms an antigen specific receptor on mature B cells - consequently has no known effector function (don’t kill antigens, purely a receptor) (IgM as a monomer can also do this)

IgE
Extra rigid central domain
has the most carbohydrates
IgE primarily defends against parasitic invasion and is responsible for allergic reactions.
basophils and tissue mast cells express very high affinity Fc receptors for IgE - mast cells then release histamine
so high that almost all IgE is bound
sensitizes (activates) mucosal cells and tissues
protects against helminth parasites
IgE’s main purpose is to protect against parasites but due to improved sanitation these are no longer a prevalent issue across most of the world. Consequently it is thought that they become over activated and over sensitive while looking for parasites and start reacting to eg pollen and causing allergies.

IgA
Exists in serum in both monomeric (IgA1) and dimeric (IgA2) forms (dimeric when 2 Fcs bind via secretory complex)
15% of the total serum Ig.
4-7 day half life
Secretory IgA2 (dimer) = primary defense against some local infections
Secreted as a dimer in mucous (e.g., saliva, tears)
prevents passage of foreign substances into the circulatory system


Isotype: class of antibody (IgD, IgM etc)
Allotype: person specific alleles
Idiotype: (hyper) variable region - antibody specificity
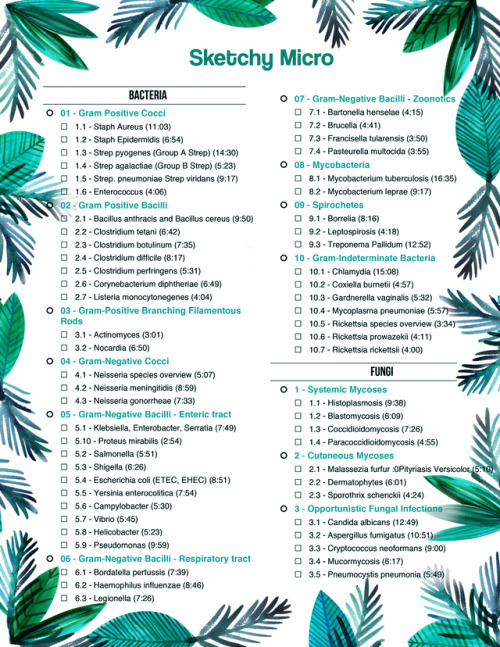
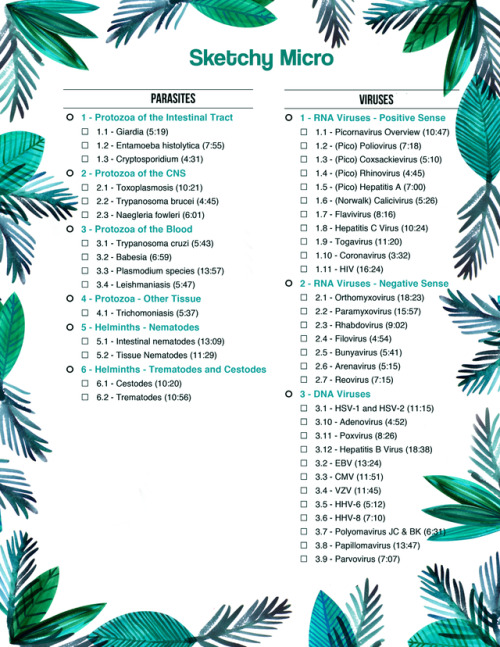
Sketchy Micro To Do List:
• 01 - Gram Positive Cocci o 1.1 - Staph Aureus (11:03) o 1.2 - Staph Epidermidis (6:54) o 1.3 - Strep pyogenes (Group A Strep) (14:30) o 1.4 - Strep agalactiae (Group B Strep) (5:23) o 1.5 - Strep. pneumoniae Strep viridans (9:17) o 1.6 - Enterococcus (4:06) • 02 - Gram Positive Bacilli o 2.1 - Bacillus anthracis and Bacillus cereus (9:50) o 2.2 - Clostridium tetani (6:42) o 2.3 - Clostridium botulinum (7:35) o 2.4 - Clostridium difficile (8:17) o 2.5 - Clostridium perfringens (5:31) o 2.6 - Corynebacterium diphtheriae (6:49) o 2.7 - Listeria monocytonegenes (4:04) • 03 - Gram-Positive Branching Filamentous Rods o 3.1 - Actinomyces (3:01) o 3.2 - Nocardia (6:50) • 04 - Gram-Negative Cocci o 4.1 - Neisseria species overview (5:07) o 4.2 - Neisseria meningitidis (8:59) o 4.3 - Neisseria gonorrheae (7:33) • 05 - Gram-Negative Bacilli - Enteric tract o 5.1 - Klebsiella, Enterobacter, Serratia (7:49) o 5.10 - Proteus mirabilis (2:54) o 5.2 - Salmonella (5:51) o 5.3 - Shigella (6:26) o 5.4 - Escherichia coli (ETEC, EHEC) (8:51) o 5.5 - Yersinia enterocolitica (7:54) o 5.6 - Campylobacter (5:30) o 5.7 - Vibrio (5:45) o 5.8 - Helicobacter (5:23) o 5.9 - Pseudomonas (9:59) • 06 - Gram-Negative Bacilli - Respiratory tract o 6.1 - Bordatella pertussis (7:39) o 6.2 - Haemophilus influenzae (8:46) o 6.3 - Legionella (7:26)
• 07 - Gram-Negative Bacilli - Zoonotics o 7.1 - Bartonella henselae (4:15) o 7.2 - Brucella (4:41) o 7.3 - Francisella tularensis (3:50) o 7.4 - Pasteurella multocida (3:55) • 08 - Mycobacteria o 8.1 - Mycobacterium tuberculosis (16:35) o 8.2 - Mycobacterium leprae (9:17) • 09 - Spirochetes o 9.1 - Borrelia (8:16) o 9.2 - Leptospirosis (4:18) o 9.3 - Treponema Pallidum (12:52) • 10 - Gram-Indeterminate Bacteria o 10.1 - Chlamydia (15:08) o 10.2 - Coxiella burnetii (4:57) o 10.3 - Gardnerella vaginalis (5:32) o 10.4 - Mycoplasma pneumoniae (5:57) o 10.5 - Rickettsia species overview (3:34) o 10.6 - Rickettsia prowazekii (4:11) o 10.7 - Rickettsia rickettsii (4:00) • Fungi • 1 - Systemic Mycoses o 1.1 - Histoplasmosis (9:38) o 1.2 - Blastomycosis (6:09) o 1.3 - Coccidioidomycosis (7:26) o 1.4 - Paracoccidioidomycosis (4:55) • 2 - Cutaneous Mycoses o 2.1 - Malassezia furfur :0Pityriasis Versicolor (5:10) o 2.2 - Dermatophytes (6:01) o 2.3 - Sporothrix schenckii (4:24) • 3 - Opportunistic Fungal Infections o 3.1 - Candida albicans (12:49) o 3.2 - Aspergillus fumigatus (10:51) o 3.3 - Cryptococcus neoformans (9:00) o 3.4 - Mucormycosis (6:17) o 3.5 - Pneumocystis pneumonia (5:49)
• Parasites • 1 - Protozoa of the Intestinal Tract o 1.1 - Giardia (5:19) o 1.2 - Entamoeba histolytica (7:55) o 1.3 - Cryptosporidium (4:31) • 2 - Protozoa of the CNS o 2.1 - Toxoplasmosis (10:21) o 2.2 - Trypanosoma brucei (4:45) o 2.3 - Naegleria fowleri (6:01) • 3 - Protozoa of the Blood o 3.1 - Trypanosoma cruzi (5:43) o 3.2 - Babesia (6:59) o 3.3 - Plasmodium species (13:57) o 3.4 - Leishmaniasis (5:47) • 4 - Protozoa - Other Tissue o 4.1 - Trichomoniasis (5:37) • 5 - Helminths - Nematodes o 5.1 - Intestinal nematodes (13:09) o 5.2 - Tissue Nematodes (11:29) • 6 - Helminths - Trematodes and Cestodes o 6.1 - Cestodes (10:20) o 6.2 - Trematodes (10:56)
• Viruses • 1 - RNA Viruses - Positive Sense o 1.1 - Picornavirus Overview (10:47) o 1.2 - (Pico) Poliovirus (7:18) o 1.3 - (Pico) Coxsackievirus (5:10) o 1.4 - (Pico) Rhinovirus (4:45) o 1.5 - (Pico) Hepatitis A (7:00) o 1.6 - (Norwalk) Calicivirus (5:26) o 1.7 - Flavivirus (8:16) o 1.8 - Hepatitis C Virus (10:24) o 1.9 - Togavirus (11:20) o 1.10 - Coronavirus (3:32) o 1.11 - HIV (16:24) • 2 - RNA Viruses - Negative Sense o 2.1 - Orthomyxovirus (18:23) o 2.2 - Paramyxovirus (15:57) o 2.3 - Rhabdovirus (9:02) o 2.4 - Filovirus (4:54) o 2.5 - Bunyavirus (5:41) o 2.6 - Arenavirus (5:15) o 2.7 - Reovirus (7:15) • 3 - DNA Viruses o 3.1 - HSV-1 and HSV-2 (11:15) o 3.10 - Adenovirus (4:52) o 3.11 - Poxvirus (8:26) o 3.12 - Hepatitis B Virus (18:38) o 3.2 - EBV (13:24) o 3.3 - CMV (11:51) o 3.4 - VZV (11:45) o 3.5 - HHV-6 (5:12) o 3.6 - HHV-8 (7:10) o 3.7 - Polyomavirus JC & BK (6:31) o 3.8 - Papillomavirus (13:47) o 3.9 - Parvovirus (7:07)

Sooo I’m studying microbiology 2:28 am because I’m a desperate bitch Microbiology + immunology = total final grade I got a 10 in my immunology test so I’m PRAYING for a 10 in microbiology so I can get a bIG BeauTiFul 10 on my final

Side effects of drugs commonly given to the elderly
For sleep aid do not give barbituates or diphenhydramine (1st gen antihistamine). Instead, give Ramelteon.
Neisseria gonorrhoeae


PMN filled with Neisseria gonorrhoeae => Gram- diplococci, glucose fermenter, non maltose fermenter, oxidase positive.
Very inflammatory response: exudate with high number of PMN. TX with ceftriaxone and always ALWAYS test for Chlamydia trachomatis (since is more common and exudate is similar)
How to tell them apart?
N. gonorrhoeae’s exudate is more purulent than C. trachomatis.
N. gonorrhoeae’s exudate is “greenish-yellowish” but C. trachomatis’s is whiter.
N. gonorrhoeae is always inside a PMN while C. trachomatis is not

Grows in Thayer-Martin medium (chocolote agar + antibiotics, is a selective medium)
Tularemia as a biological weapon
It was viewed as an attractive agent because:
it is easy to aerosolize,
it is highly infective; 10-50 bacteria are required to infect,
it is nonpersistent and easy to decontaminate (unlike anthrax),
it is highly incapacitating to infected persons,
it has comparatively low lethality, which is useful where enemy soldiers are in proximity to noncombatants, e.g. civilians
can you see the irony……we are working our ass off to kill these bugs.At th same time some weirdo working in one lab is making bio weapon.


black and white checklist for sketchy micro
Dose Dependent effects of Dopamine mnemonic

Simplified version of Dopamine’s dose-dependent MAJOR effects:
low doses - activates D1 receptors (Gs) - vasodilates renal blood vessels*
med.doses - activates B1 receptors (Gs) - increases heart rate/contractility etc..
high doses - activates A1 (Gq) - vasoconstricts,
*increased renal perfusion, GFR, also vasodilates mesenteric and coronary vessels
source: http://reference.medscape.com/drug/intropin-dopamine-342435
Passive Immunotherapy
Active immunotherapies:
Cytokines (TNFa IL-2, IFNs)
Cancer vaccines
tumour CTL and APC
DC priming
Passive immunotherapy:
Administration of monocolnal (clone derived asexually from a single individual or cell) antibodies which target either tumour-specific or over expressed antigens
Generally comprised of antibodies made outside of the body (in a lab)
administered to patients to provide immunity against a disease, or to help fight existing disease
do not stimulate a patient’s body to ‘actively’ respond to a disease the way a vaccine does
immunogen is given several times to induce a strong secondary response
blood serum contains many different antibodies to the immunogen
most immunogens have multiple antigenic epitopes
each stimulates a different B cell clone/receptor –> polyclonal antibody (PAb) response

Monoclonal antibody (mAb) therapy is the most widely used form of cancer immunotherapy. Monoclonal antibodies cannot be purified from a polyclonal sample and are derived from a single clone/specific for a single epitope.

Antibodies in cancer therapy:
Trigger immune system to attack cancer cells
Block molecules that stop the immune system working (checkpoint inhibitors)
Block signals telling cancer cells to divide
Carry drugs or radiation to cancer cells
Checkpoint inhibitors
Immune system uses particular molecules to stop it being over activated and damaging healthy cells - these are known as checkpoints
some cancers make high levels of checkpoint molecules to switch of immune system T cells which would normally attack cancer cells
examples of targets include CTLA-4, PD-1 and PD-L1 (programmed death ligand 1)

Blocking cell division signals
Cancer cells often express large amounts of growth factor receptors on their surface –> rapid cell division when growth factors stimulate them
some monoclonal antibodies stop growth factor receptors working
either by blocking the signal or the receptor itself
cancer no longer gets signal to divide

Carrying drugs/radiation
drugs or radioisotopes can be attached to monoclonal antibodies
the mAB binds to the cancer cell, delivering directly
known as conjugated MABs

-
 nodramaqween liked this · 1 year ago
nodramaqween liked this · 1 year ago -
 loveforneurosurgery reblogged this · 1 year ago
loveforneurosurgery reblogged this · 1 year ago -
 loveforneurosurgery liked this · 1 year ago
loveforneurosurgery liked this · 1 year ago -
 yahajbaba liked this · 1 year ago
yahajbaba liked this · 1 year ago -
 bacilost reblogged this · 1 year ago
bacilost reblogged this · 1 year ago -
 step1studying liked this · 2 years ago
step1studying liked this · 2 years ago -
 lela4 liked this · 3 years ago
lela4 liked this · 3 years ago -
 doctornimsblog reblogged this · 3 years ago
doctornimsblog reblogged this · 3 years ago -
 ryuk10101010101 reblogged this · 3 years ago
ryuk10101010101 reblogged this · 3 years ago -
 ryuk10101010101 liked this · 3 years ago
ryuk10101010101 liked this · 3 years ago -
 fague liked this · 3 years ago
fague liked this · 3 years ago -
 the24hrtherapist liked this · 3 years ago
the24hrtherapist liked this · 3 years ago -
 studikins liked this · 3 years ago
studikins liked this · 3 years ago -
 strangeflowerhumanoiddonkey liked this · 4 years ago
strangeflowerhumanoiddonkey liked this · 4 years ago -
 raconteur-k liked this · 4 years ago
raconteur-k liked this · 4 years ago -
 paureus reblogged this · 5 years ago
paureus reblogged this · 5 years ago -
 devinfreetime liked this · 5 years ago
devinfreetime liked this · 5 years ago -
 saimani1997 liked this · 5 years ago
saimani1997 liked this · 5 years ago -
 angelaellar reblogged this · 5 years ago
angelaellar reblogged this · 5 years ago -
 the-bell-jar-illiteracy reblogged this · 6 years ago
the-bell-jar-illiteracy reblogged this · 6 years ago -
 puppapzzy reblogged this · 6 years ago
puppapzzy reblogged this · 6 years ago -
 zekarichan liked this · 6 years ago
zekarichan liked this · 6 years ago -
 tblack34 liked this · 6 years ago
tblack34 liked this · 6 years ago -
 duanegod-blog liked this · 6 years ago
duanegod-blog liked this · 6 years ago -
 eliena1234 liked this · 6 years ago
eliena1234 liked this · 6 years ago -
 dokiemg reblogged this · 6 years ago
dokiemg reblogged this · 6 years ago -
 t-b-a-blr-blog reblogged this · 6 years ago
t-b-a-blr-blog reblogged this · 6 years ago -
 t-b-a-blr-blog liked this · 6 years ago
t-b-a-blr-blog liked this · 6 years ago -
 superspypeanutjudge-blog liked this · 6 years ago
superspypeanutjudge-blog liked this · 6 years ago -
 nukeeeeeeeeeee-blog reblogged this · 7 years ago
nukeeeeeeeeeee-blog reblogged this · 7 years ago -
 yanismichelle liked this · 7 years ago
yanismichelle liked this · 7 years ago -
 onshchk-blog reblogged this · 7 years ago
onshchk-blog reblogged this · 7 years ago -
 poisonnightmares liked this · 7 years ago
poisonnightmares liked this · 7 years ago -
 med-wonderland liked this · 7 years ago
med-wonderland liked this · 7 years ago -
 sessizbimelek reblogged this · 7 years ago
sessizbimelek reblogged this · 7 years ago -
 aakritiu liked this · 7 years ago
aakritiu liked this · 7 years ago -
 3rdyearsucks-blog reblogged this · 7 years ago
3rdyearsucks-blog reblogged this · 7 years ago -
 unorthodoxjoh liked this · 7 years ago
unorthodoxjoh liked this · 7 years ago -
 mystudynotes5-blog reblogged this · 7 years ago
mystudynotes5-blog reblogged this · 7 years ago -
 rainbowsnsunshines liked this · 7 years ago
rainbowsnsunshines liked this · 7 years ago -
 e-aezea liked this · 8 years ago
e-aezea liked this · 8 years ago -
 ferlistudyblr reblogged this · 8 years ago
ferlistudyblr reblogged this · 8 years ago -
 ferlizavala liked this · 8 years ago
ferlizavala liked this · 8 years ago -
 zhuykay-blog reblogged this · 8 years ago
zhuykay-blog reblogged this · 8 years ago -
 cindyruth-blog1 liked this · 8 years ago
cindyruth-blog1 liked this · 8 years ago -
 darshk-blog1 liked this · 8 years ago
darshk-blog1 liked this · 8 years ago -
 xcvish liked this · 8 years ago
xcvish liked this · 8 years ago -
 paolocabeza-blog liked this · 8 years ago
paolocabeza-blog liked this · 8 years ago